When we stand up, gravity shifts blood toward the lower body, reducing the amount of blood returning to the heart. The nervous system initiates rapid reflexes to counteract gravity-induced effects, and dysfunction of this neural compensation can lead to postural hypotension, a sustained decrease in blood pressure that causes dizziness or fainting. However, the specific neural pathways that detect posture-related changes in circulation have been difficult to disentangle.
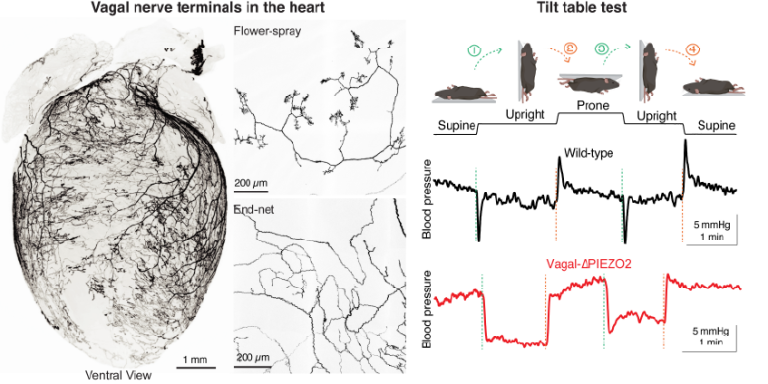
In this study published in Nature, the Liberles Lab identified a small population of vagal sensory neurons that innervate the heart and act as blood volume receptors. These neurons express the mechanosensitive ion channel PIEZO2 and form distinctive end-net endings in the heart. Using mouse tilt-table experiments, anatomical mapping, in vivo electrophysiology and calcium imaging, and targeted genetic gain/loss-of-function approaches, the team shows that this vagal pathway is required for normal compensation to upright posture.
Notably, the identified vagal PIEZO2 neurons produce heartbeat-coupled signals that track central blood volume and are time-locked to phases of the cardiac cycle. Selective knockout of PIEZO2 eliminates this heartbeat-coupled activity, causes postural hypotension, and compromises cardiovascular stability during trauma-induced blood loss. The work also demonstrates that optogenetic stimulation of these vagal fibers can lower blood pressure, supporting a causal role in hemodynamic control.
Together, these findings reveal an essential vagal reflex that defends the constancy of circulation during posture change and hemorrhage, expanding our understanding of heart-brain communication in cardiovascular homeostasis.